Ted’s Relapsing PolychondritisOctober 15, 2007
|
| Symtoms | |
|---|---|
| #1 & #2 #3 #4 #5 #6 & #7 |
10 to 15 minutes 15 to 20 minutes 30 to 40 minutes 40 to 50 minutes 1 to 1½ hour |
I understand that various steroids, whether oral or injected, can control the laryngotracheal symptoms caused by an inflammatory response from RPC. However, I know that such medications usually have negative side effects, especially when used over a prolonged period of time. As such, I would rather not use steroids on a long-term basis. If no other medical treatment is available to me, I would prefer to continue attempting to manage my symptoms by breathing through filters.
Lacking any other explanation, it seems that some substance, commonly found in the fabric of carpeting and maybe some furniture, is “triggering” an immune response to the cartilage in my larynx and trachea whenever I inhale the substance. Another possibility is that antibodies have changed the cartilage in my larynx and traches to such an extent that some substance in carpeting irritates those structures when inhaled. Honestly, I have no idea how nor why this occurs, nor have I found another case like mine while searching the web; I only can speculate.
In any case, I am wondering if there might be any way to detect and to identify this substance. If so, I wonder if it would be possible, considering that my body may perceive this substance as some type of antigen, to create an injectible serum that would desensitize my immune system or my laryngotracheal cartilage to this substance.
I will be seeing an immunologist/allergist in a few weeks, but I am not really getting up my hopes. If I am to continue having this problem, then I believe it is God’s will for that to be the case, and I am OK with that. People will just have to understand that I need to wear my masks and filter contraptions in their homes. If not, then I won’t go there. So far, my family and friends have been very understanding and accepting.
There is a reason for everything, even death. It may be that my cardiac and laryngotracheal signs/symptoms are end-stage phases of my RPC disease. So if my heart suddenly stops, or if my trachea ultimately collapses and I suffocate, then I’ll go to an infinitely better place, and I will be happy there. I have no expectation or anticipation of a miracle, although I absolutely do believe that such an event is possible. Whatever has been predestined by the Lord—not just for me, but for all of us—will take place. ![]()
November 21, 2007
I saw an allergist/immunologist doctor today. I had mailed him a letter over a month ago explaining my symptoms, and I also had included my lab test reports. He indicated that he had read everything and also had researched my condition. Although he’d never seen anyone with my disorder before, he agreed that Relapsing Polychondritis most likely is what I have. He said that my symptoms and affected body parts definitely “fit the pattern.”
Incidentally, he did an extensive regimen of testing for allergies to all types of substances. I was allergic to absolutely nothing, which did not surprise me. I never have had allergy problems in my life.
The doctor also agreed that steroids probably are the only medication that can control my symptoms. However, as I knew, long-term use of steroids can compromise my immune system, leaving me vulnerable to various infections. Besides that, steroids can have several other adverse side-effects.
December 5, 2007
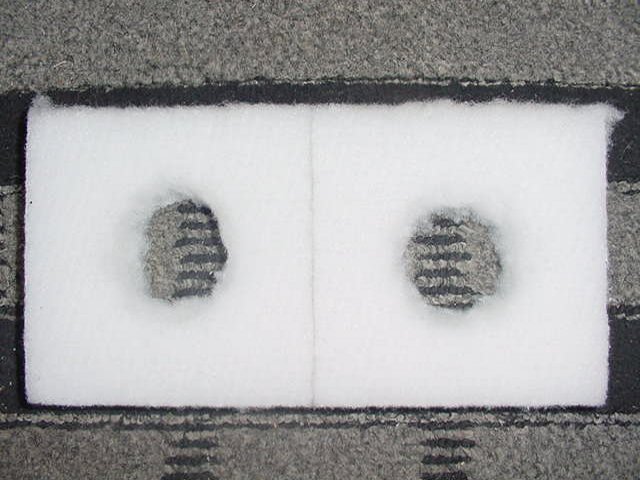
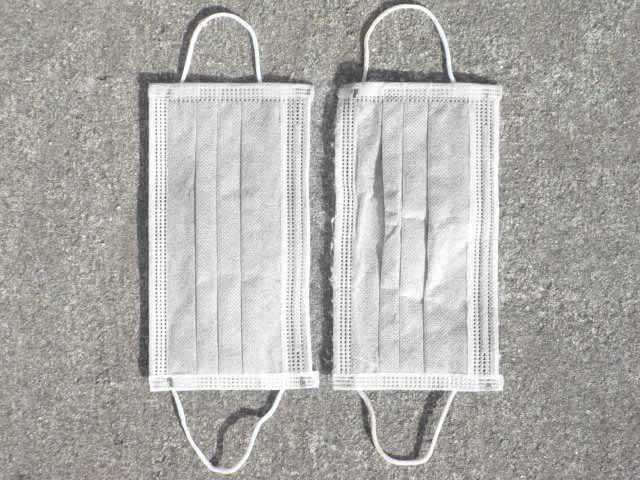
Wearing my masks, which I must do all the time when I am inside a house or apartment (and some other places, especially with carpeting) is very inconvenient, awkward and problematic for me. I wear two surgical masks over my nose and mouth, with loops which hook over my ears. One mask does not work as well as two masks do in relieving my symptoms. Sometimes I need to have an extra dust or paint mask over these.
This makes common activities such as eating, drinking, shaving, brushing my teeth and showering quite awkward. If I inhale any room air, either through my nose or mouth, while doing these things, then my uncomfortable symptoms will begin, before long. It is a significant hassle that I simply have to live with.
I have had trouble locating the type of surgical masks that function as adequate filters. I ordered 600 masks online, only to discover that they were too thin and were almost like wearing nothing at all. Evidently, there is a difference between “procedure” masks (which I bought) and “surgical” masks (which are thicker and work pretty well).
Below, the purple and yellow masks on the left are “surgical” masks. The blue mask on the right is a “procedure” mask. Other than the colors, they all look the same, don’t they? Well, they’re not. The first two masks work well for me, but the third mask is worthless.
However, for the first two masks to work, I have to rinse them, soak them overnight in distilled water, rinse them again, soak them overnight again, and often rinse them and soak them overnight for a third time. Then I have to hang them somewhere to dry, usually overnight. Evidently, the masks are treated with something which actually brings on my breathing symptoms. Once I rid the masks of whatever that substance is, they work for me.
I have been able to obtain some surgical masks through friends working at health facilities, as well as from my dentist’s office. But I’d like to find a large, inexpensive batch of them to purchase. It sure would help relieve some of my frustration and aggravation.

The type of mask pictured below is effective in relieving my breathing symptoms. Also, it doesn’t seem to be treated with anything that exacerbates my symptoms. However, I don’t like having the elastic band over my head all day long; so I prefer to wear the other masks, once they have been adequately soaked and dried.

March 23, 2008
Resurrection Day
For about a week, I have been experiencing quite a bit of pain in my larynx (“voice box”). Also, my voice has been hoarse and raspy. I suspect that the cartilage in my larynx is being attacked by my antibodies.
This next week, I intend to shut down my talking by about 90%. I may have to stop talking altogether—although that would be quite difficult to do, as far as being able to communicate with other people—if this does not significantly reduce the pain and help my voice return to normal.
May 3, 2008
For a few weeks, I have been noticing pain in my left hip when I wake up during the night, after having been sleeping on my left side. There also has been pain in my right hip as well, after sleeping on that side, but not nearly as much as in the left hip. I have placed two full-length pillows on either side of me in bed, and I make sure that I rest my upper thigh on the bottom corner nearest me of whatever pillow is in front of me when I turn over. This seems to “suspend” each hip, somewhat, so that it is not being pressed as hard into the mattress. As long as I do this, I can sleep with less hip pain.
My hips (especially the left one) also hurt after sitting for awhile. So I have increased my Glucosamine and Chondroitin intake each day to 1½ tablets, each containing 1,500 mg Glucosamine and 1,200 mg Chondroitin. Sometimes (not everyday) I also dissolve ½-teaspoonful (3,000 mg) of powdered MSM into water and drink it once a day. My pain has diminished noticeably, so I will continue taking these substances everyday.
A few nights ago, I woke up with pain on the left side of my chest. Initially, I was thinking maybe it was a heart valve problem, since I had chest pains and an irregular heartbeat several times during 2005 and 2006, the longest single episode lasting for 50 minutes. (Heart valves contain cartilage.) I am thinking my recent pain is a rib problem (most ribs are connected to the sternum with cartilage), since I experience the pain primarily when I have slept on my left side, just like my hip pain.
Now I rest my rib cage on the upper part of the pillow at my side, and that diminishes the level of pain. Oh yeah, and I still have to make sure my masks don’t slide off, and also minimize pressure on my ears while I am sleeping. It’s all a fine-tuned “balancing act” to be able to sleep at night.
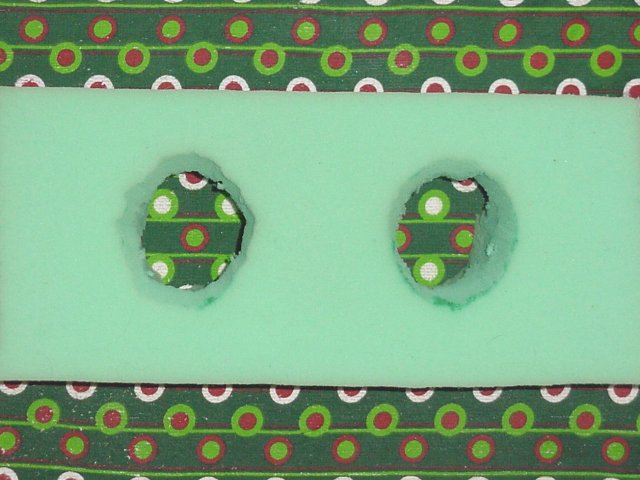
Sometimes I sleep with my head on a seat cushion, with four indentations. My ears fit into the indentations. I have better success without a pillow case. However, over time, the pillow loses its firmness, my ears touch the bottom of the indentations, and I experience ear pain and temporary deafness whenever I wake up.

The increase in intake of all of those chemicals seems to have helped reduce my rib pain, to some extent, as well. Of course, I’d rather not be consuming them, but at least they are better than taking corticosteroids, which probably would have way too many negative side effects. I have read that some people with RPC eventually need to have complete hip and knee replacements. I hope I never have to deal with that. Relapsing Polychondritis is a hassle. Ugh!
June 7, 2010
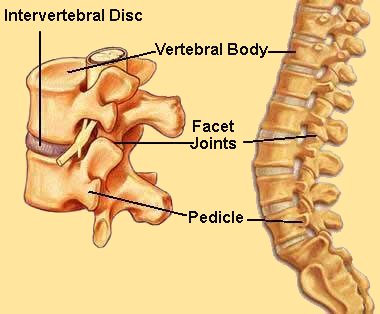 A week ago, I lifted something heavy. A few days later, I began having really bad pain in my lower back. I think I have a herniated disc, and the pain has been present everyday since. The intervertebral discs are fibrocartilaginous cushions serving as the spine’s shock absorbing system, which protect the vertebrae. Since these discs contain cartilage, they can be prone to herniating more easily in someone with RPC.
A week ago, I lifted something heavy. A few days later, I began having really bad pain in my lower back. I think I have a herniated disc, and the pain has been present everyday since. The intervertebral discs are fibrocartilaginous cushions serving as the spine’s shock absorbing system, which protect the vertebrae. Since these discs contain cartilage, they can be prone to herniating more easily in someone with RPC.
I found a fixed, horizontal bar and hung upside down on it several times, for about 10 seconds at a time (otherwise, I would get too dizzy). That seems to have helped the pain, probably by pulling the vertebrae apart a little and reducing the pressure on my affected disc (if that is what the problem is). In the future, I will need to be aware and careful not to lift anything too heavy.
April 1, 2011
Since making my last entry on June 7, 2010, I have kept almost everything the same, as far as relieving my RPC symptoms. I still sleep with my head on a foam rubber pillow with holes cut into it to eliminate any pressure on my ears. I take 1¼ tablets per day containing both Glucosamine and Chondroitin, with each tablet containing 1,500 mg Glucosamine and 1,200 mg Chondroitin. That seems to keep my knee, hip, rib and lower back pain under control, for the most part.
I have not had any new episodes of severe lower back pain like I did at the beginning of June. That pain gradually subsided, over a few weeks, and bothers me only a minimal amount now. I do have twinges of back pain within a day after I lift something that I probably shouldn’t have lifted, but I never lift anything really heavy anymore. I do not want to take a chance on doing any further damage to my lower back.
As of yet, I have not taken prescribed medications for my condition. I’d rather not deal with the negative side-effects of steroids, Methotrexate, or anything else that I might take to relieve my symptoms.
Recently, I had an episode of bronchitis, which lasted several days. It would have lasted longer, had I not been popping penicillin day and night for over a week. Soon after my bronchitis had improved significantly, I unexpectedly lost 7 pounds over a one-week period, even though I was eating normally. I can gain back as much as 2 pounds, but then I will lose what I gained. This appears to be my new plateau, which is fine with me as long as I do not lose more weight.
RPC can cause weight loss. What I suspect happened is that my bout with bronchitis caused my RPC to worsen, resulting in a relapse (which is how Relapsing Polycondritis gets its name). Also, since then, I have been even more sensitive to carpeting than I was before, and now I have to wear three surgical masks (or two surgical masks and a paint mask) to control my breathing problems. Three masks definitely are more inconvenient than two masks, so I hope that this aspect of my condition improves over time.
I have to wear the masks whenever I am inside my house, since carpeting is present. The thing is that most masks, right out of the box, seem to be coated with some substance that triggers my breathing problems. Therefore, I usually have to soak my masks for several days in distilled water, rinse them well, then hang them up to dry, before I can use them. Sometimes I have to repeat the soaking/drying process two or three times before the masks are effective.
If I am in another place besides my home that has carpeting, and if I do not have my masks, I hold a napkin, tissue, a washcloth or something else over my nostrils to filter out whatever it is that causes my breathing difficulties. As long as I am able to breathe normally, my heart rate is normal as well, and I rarely have heart palpitations or spikes in blood pressure. If I am outside, I have no problems breathing at all, since I do not have common allergies that many people are plagued with.
From the emails I have received from people who have RPC, it seems that I am in a small minority of people who experience breathing difficulties while around carpeting. It doesn’t matter whether the carpeting is new, old, clean, or dirty. I do not know why, after 2-10 minutes, it causes me to feel like I have inhaled something toxic and noxious, at which time I will begin to cough. It is extremely uncomfortable.
I will do just about anything to avoid that burning, painful sensation, which just gets worse if I keep breathing unfiltered air near carpeting. Since RPC sufferers have some variability in their symptoms, and in the severity of their problems, I don’t think that many of them have the same difficulties that I do when I am around carpeting. But then I do not have some of the same symptoms and problems that they do, either.
Anyway, I hope and pray that others with RPC are successful in finding things that will help control their symptoms. For me, praying to God/Yahweh has resulted in my finding beneficial solutions that I probably would not have discovered otherwise.
April 15, 2011
I have developed a new symptom in the past two weeks since I made my last entry. I am assuming that it is another “relapsing” symptom (from which Relapsing Polychondritis or RPC gets its name) caused by my bout with bronchitis last month, as explained in my entry of April 1.
Infections cause the body to produce antibodies, in an attempt to neutralize the foreign invader. In my case, though, this process also seems to cause my body to produce antibodies that target additional body tissues (usually, but not always, cartilage), which are harmless but my body mistakenly sees them as invaders. It is a misdirection of the immune system.
My new symptom is reduced vision in both eyes but mainly in my right eye. For over a week, I did not make the connection to my RPC. However, once it occurred to me that this was a possibility, I searched the internet for a potential correlation and found this case report:
Corneal autoimmunity in a patient with relapsing polychondritis
In short, the article indicates that in someone with RPC, antibodies against the corneal epithelium (the most anterior or outer layer of the cornea) can be present. Indeed, the corneal epithelium of my right eye seems to be affected the most.
Previously, after wearing and removing my contact lenses, my visual acuity was perfect (20/15+ with each eye) using glasses. Now, after contact lens removal, the vision in my left eye is slightly blurred and the vision in my right eye is very blurred with glasses. It takes only an hour or so for the acuity in my left eye to return to normal; however, the acuity in my right eye remains noticeably blurry for days.
Even when my right eye acuity is relatively clear, after several days of not wearing contact lenses, I continue to notice a “ghost image” below the main image with my right eye. This “ghost image” has not gone away. Evidently, when my lenses rub up and down against my corneal epithelium, it causes antibodies to migrate to the area and distort my epithelium. It may be similar to how my ears become beet red after being pressed into a pillow for awhile. Unfortunately, it looks like I may not be able to wear contacts anymore. I do not want to take the chance of decreasing the visual acuity anymore in either eye.
Also, I have to be very cautious about being around sick people and crowds where people might be sick. I have to do everything I can not to catch any “bugs.” Whenever I do, my RPC symptoms get worse.
June 15, 2011
I have lost 12 pounds in two months. That might not be so unusual except that the first five pounds were in less than a week (in April), and the next seven pounds were in about a week recently (early June). I have not changed my eating habits at all, and my appetite is normal, although I am having mild abdominal discomfort and some rumblings a few hours after eating. Also, I was not overweight to begin with; I was at pretty much my optimum weight.
At this point, I am suspecting that my RPC may be causing Irritable Bowel Disease or something similar. This would cause less nutrients to be absorbed by my intestines and, in turn, would cause weight loss. I intend to see a doctor for further consultation, probably next month.
Last week, I found some 13" x 6" x 5" foam rubber slabs and cut holes in them with an electric knife. They are taller than my other foam slabs, so I do not need to put anything under them when I use them as pillows. I keep my ears in the holes when I sleep so that the cartilage in my ears will not become inflamed and red. So far, they are working great.
August 1, 2011
I saw a doctor recently, and he ordered blood tests. Everything is normal, except my HDL (good cholesterol) is a little low. So I will be taking more fish oil.
I have not gained any of my weight back, after having lost 12 pounds. I also recently have noticed more “rumbling” noises in my abdominal area, as well as some discomfort when I eat. Something is going on down there. I have scheduled a colonoscopy for early September.
September 18, 2011
I had a colonoscopy on September 8. During this one, and during the one I had six years ago, I chose not to be sedated. I have a pretty high tolerance for discomfort, so it was no big deal. I wanted to be wide awake to watch the whole thing on the video screen and also to ask the doctor questions while he was performing the procedure.
No cancer nor any polyps were present. Everything looked great. The doctor said he could not trace my recent weight loss to a colon problem. However, he suggested that, perhaps, I could have Celiac Sprue (that page, with six panels, may take a minute to load), which affects the small intestine. In this condition, gluten, a grain protein, damages the villi of the small intestine, causing the absorption of nutrients to be lessened. One thing this can cause is weight loss.
Gluten is found in wheat, rye, barley and possibly oats. I hardly ever eat bread or foods containing grains, but I do eat raw oats almost everyday. I went a day without oats, and my stomach still felt unsettled after eating. The next day I added my oats, and I didn’t get the unsettled feeling. I am not convinced that I have Celiac Sprue, but I suppose it’s possible. I’m still experimenting.
A friend suggested that I eat a lemon a day, which I have done almost everyday since my colonoscopy. I cut a lemon in quarters and eat all four slices, one by one, including the skins. Interestingly, I have had little to no unsettled feeling on days that I have eaten a whole lemon. Also, my weight seems to have leveled out, at least for the time being.
November 17, 2011
Today, my Relapsing Polychondritis made a giant leap for the worse, as far as my breathing is concerned. Usually a worsening of my RPC occurs soon after having some type of upper respiratory or other infection; but I have not had such an infection for about eight months, so I can see no direct cause of this.
Up until now, I have been able to eliminate most or all of the irritation and burning in my trachea (windpipe) by wearing surgical masks over my nose. I have worn them when I am around carpeting and some rugs because the masks adequately have filtered out whatever it is that triggers my breathing difficulties (which still remains unknown). Now, however, no amount of filtering the air I am breathing seems to eliminate the problem, although it is even worse if I remove my masks altogether inside of a carpeted room, which has been the case since 2007.
Furthermore, while wearing my masks, I have been measuring my blood pressure at about 145/95 (and as high as 150/102), even though it previously has been normal at about 120/70. Also, my heart rate has been about 75-78 bpm, even though it typically is about 63-65. These values are much too high for me. Fortunately, my weight seems to have stabilized, which is good.
November 24, 2011
Today I woke up before dawn with my heart pounding, and at times it was irregular (skipping beats). My heart rate was 87 bpm. Usually, it is about 54 bpm early in the morning while I am still in bed.
Also, when I got up and looked in the mirror, I could see that both ears were red, even though I had been sleeping properly on my green pillow with holes in it. Furthermore, my hearing is mildly decreased in both ears. Evidently, my body is becoming increasingly stressed due to the effects of the Relapsing Polychondritis.
Over the past week, I have experienced an increasing amount of burning and irritation in my trachea (windpipe), virtually 24 hours a day. Wearing masks in a carpeted room, which I have done for over four years, only slightly alleviates my breathing problems now but does not eliminate them anymore.
Yesterday and today, I also have been coughing and experiencing hoarseness. Evidently, the cartilage in my larynx is being compromised as well. All of this is very uncomfortable, and I am feeling pretty anxious and apprehensive about it.
If I cannot get this under control, I estimate my survival rate right now to be about 50%. At some point, it is possible that my trachea will tear or collapse, and then I probably will suffocate. I’m not sure what to do. Notwithstanding all of this, though, it is Thanksgiving and I still am thankful for all of my many blessings.
December 1, 2011
I am staying with friends whose second floor has no carpeting. I can sleep, eat and work on my computer up here. I still need to wear my masks, though; otherwise, my breathing problems begin. Maybe there are residual carpet fibers from downstairs that float upstairs or something, but my masks are effective as long as I do not have carpeting directly under me.
I found and ordered a few charcoal filter masks online. They are supposed to filter out 99% of everything. I now am wearing a paint mask with an elastic band (which I don’t really like wearing, but the mask is effective), a charcoal filter mask and a couple of folded napkins. Maybe this combination will enable me to be on a carpeted floor again. I hope this significant relapse in my condition doesn’t last too much longer.
January 1, 2012
After my severe degree of tracheal inflammation finally subsided, following the use of my most recent mask combination for a couple of weeks, I am able to be in a carpeted room at my friends’ house.
I have tried this mask combination at my own house, but it did not seem to work as well there. Whenever I am there, I can minimize my symptoms by using about double the number of masks, which is inconvenient but at least it works.
February 1, 2012
My recent flare-up seems to have subsided noticeably, and I now am back to using my regular masks. I can be in my own house, although I need to wear several more masks there than I do anywhere else for my breathing symptoms to be minimal. As long as I do the following things, I remain virtually free of symptoms:
- Use my masks around carpeting.
- Sleep on a foam pillow with holes in it so that there is no pressure on my ears.
- Take glucosamine and chondroitin tablets daily.
I still do not know what caused my most recent flare-up that began about 2½ months ago. In any case, I’ll just need to be extra careful not to catch a bacteria or virus that will give me a cold or upper respiratory infection. That virtually always causes my breathing difficulties to become worse for awhile.
June 15, 2012
I went on a strict diet for 2 weeks of only fruits and vegetables, no meat, no bread, no dairy, no eggs and no desserts or other sweets. I also took a probiotic capsule everyday, along with my assortment of daily vitamins. This had absolutely zero positive effect at all on my condition; none of my symptoms have improved even the slightest bit.
Incidentally, the only dairy that I consume semi-regularly is a little bit of powdered milk dissolved in filtered water. It is weaker than a normal helping of nonfat milk.
In any case, some people with autoimmune conditions evidently are helped by certain diets. Others are not. It is worth a try, though, for those who have not yet done it.
October 24, 2012
For a couple of months, I have been having intermittent inner ear aches, mild hearing loss and headaches, mostly on the left side. I finally have determined the cause. It is due to cell phone use. I very rarely use a cell phone other than to talk with a few close friends, usually briefly. When I do, I prefer using my left ear, but sometimes I use my right ear.
After ruling out possible causes for my inner ear and head pain, I did an experiment after being pain-free for a few days. I used a cell phone for 10 minutes, mostly on my left ear but about a minute on my right ear. In less than half an hour, I could feel the pain beginning in my left inner ear. The pain gradually became worse, and then I began feeling pain in my right inner ear as well.
After a couple of hours, the pain was much worse in my left inner ear. I also had a headache on the left side and felt pain behind my left eye. The pain lasted throughout the night. The next morning, all of the pain had improved somewhat, but my hearing in my left ear was decreased by about 50%. It took a couple of days for all the pain to go away and for my hearing to be completely restored.
Today I put the cell phone in speaker mode and placed it a couple of feet away from me; then I made a 5-minute phone call. After a couple of hours, I noticed mild inner ear pain on both sides, but a little more on the left. Evidently, the radiation from the phone, even at that distance, has an adverse effect on my inner ears. I probably will eliminate all cell phone use, except in emergency situations.
April 20, 2013
I have not used a cell phone much for the past several months. Everytime I did, I experienced inner ear pain. Although this occurred to a lesser extent in speaker phone mode, it still happened.
Recently, though, I noticed that the inner ear pain was almost nonexistent when I used the cell phone a few times, even when I held it up to my ears. Now, amazingly, there seems to be virtually no pain at all with cell phone use. So I may increase my usage.
This seems to be a pattern with RPC. New symptoms will flare up out of nowhere and last for awhile, often weeks to months, and then subside. But at any time, they may relapse again and even be joined by new symptoms.
I still must continue to wear my masks, or place a washcloth or other filter over my nose, when carpeting is underneath me. As long as I do this, I am fine. I also continue taking chondroitin and glucosamine; these mostly keep my hip, knee and joint pain under control.
May 20, 2014
Although I have not made an entry on this page for 13 months, I’m still around. I continue to have no ear pain after using a cell phone.
Over the past couple of months, though, I have lost 13 pounds without trying. It is similar to what I described in my June 15, 2011 entry. That resolved after several months, and I gained back all of my weight. Now that problem is back, although I am not having any of the abdominal discomfort or rumblings that I was experiencing last time.
Also, I am more limited in the masks that work to filter whatever it is (in carpeting) that causes my breathing difficulties. For years, I have not been able to pull a mask, or a couple of masks, directly out of a box and wear them successfully. All masks seem to be treated with something that triggers an inflammatory reaction in my trachea.
So I have to wash, soak and dry several masks, usually repeatedly, before a few of them work for me. It’s strange that for two seemingly identical masks out of the same box, having undergone the same amount of washing, soaking and drying, one of them will work fine, while the other does not work at all and I will feel breathing discomfort with it within 2-3 minutes. It is a mystery. Anyway, now there are fewer masks that will work adequately for me after I wash, soak and dry them.
Finally, I have a new symptom that I’ve never had before. In mid-April, I began having mild to moderate pain in the middle of my back. Since then, the area of pain has gone up and down a few inches. On a 1-10 pain scale, it ranges from a 1 to a 6. Aspirin or ibuprofen helps for awhile, and then the pain returns.
I am guessing that my RPC is affecting the discs, composed of cartilage, between my vertebrae. It is not a debilitating problem, but it is annoying and aggravating.
I continue sleeping with my head on a green foam rubber slab at home. Some people have suggested to me that the foam rubber might have a negative effect on my condition. However, I sleep without any masks (in an uncarpeted room), and I have no breathing problems at all.
If anything I inhale causes any type of inflammation in my trachea (windpipe), I notice it within a few minutes. If I am sleeping, I wake up with irritation and discomfort in my breathing passage. So the foam rubber is a neutral substance that definitely does not cause a problem for me.
If I travel, I take a blue ring “Total Pillow” (see below) that works fine. I just have to put the latter on top of a pillow to elevate my head adequately and keep my right or left ear in the hole, depending on which side I’m lying on.

July 31, 2015
On and off, for a couple of months, my immune system seems to have gone into “hyperactive” mode. During those times, my breathing problem around carpeting has been more difficult than usual, and my masks have not worked as effectively. Also, my hips and knees have hurt more than usual.
I do not know why this has happened, as I have not been sick recently. In the past, some type of illness usually seems to have been the cause of an escalation in my RPC reactions.
This past week, a doctor friend from No. CA has been visiting me, and he prescribed me some Prednisone. He has known of my relapsing polychondritis since it was diagnosed over a decade ago. I took the following amounts of Prednisone for five days:
Day #1: 40 mgThere was an improvement in my breathing, as well as in my joint pain, all five days. I even got by much of the time without using masks around carpeting.
Day #2: 20 mg
Day #3: 10 mg
Day #4: 5 mg
Day #5: 5 mg
After I stopped taking the Prednisone, my immune system seems to have calmed down and my masks are working again around carpeting. I probably would continue using Predisone on a regular basis, but I do not want to risk having to deal with the potential adverse, long-term side effects of steroidal use.
May 15, 2017
My RPC symptoms have been minimal since my last entry. This has been the case as long as I have worn a mask (or occasionally used Prednisone) around carpeting, have used a pillow that prevents pressure on my ears when sleeping and have taken my daily supplements.
It continues to be very rare that I will take Prednisone, and that’s only if I know that I am going to be in a public place for awhile where carpeting is present. I do not like to wear my masks in public because I’ve occasionally been asked, by people staring at me, if I might have something that is contagious. I do not, but I don’t like to make people nervous.
For a couple of months, I seem to have been more tired than usual and have experienced occasional mild loss of balance. I also have had intermittent tingling in my fingers, hands, toes and feet, as well as occasional variations in vision. I hope that I am not experiencing early symptoms of multiple sclerosis (MS), which is another autoimmune condition. I doubt it, but I suppose anything is possible.
August 31, 2017
My occasional mild loss of balance, intermittent tingling in my fingers, hands, toes and feet, and occasional variations in vision have dimished significantly. I don’t know why I was having those symptoms, but they seem to have resolved, at least for now. Perhaps, in time, they will return. I hope not.
October 8, 2017
I am still around and doing OK. I still have to deal with wearing masks around carpeting, but all of my other symptoms continue to be under control. My goal is to remain free of bacterial, viral, fungal and other types of infections. These seem to stimulate my immune system to produce weird, misguided antibodies that attack the cartilage in various parts of my body, resulting in another “relapse” of polychondritis. Presently, that is under control.
So if I notice the first symptom of anything (such as, for instance, a sore throat and/or a persistent cough), I immediately begin taking olive leaf extract (OLE) capsules. OLE is a miracle herb as far as I’m concerned. If taken in the earliest stage of an infection, it is an amazing “anti-everything” that, for me, can stop the problem from developing if taken for 3-4 days. Olive leaf extract can be found all over the place online or in health food stores.
April 25, 2018
Last month, my knees (especially my left knee) were becoming increasingly painful, especially when walking down stairs. My hips also started becoming pretty painful when I would lie on them during the night, and I do prefer to sleep on my sides.
A few years ago, I had cut back my daily intake of Glucosamine and Chondroitin back down to 1 tablet, each containing 1,500 mg Glucosamine and 1,200 mg Chondroitin. So I increased my daily intake back up to 1½ tablet. That reduced the pain level in my knees and hips by about half.
I have heard that Hyaluronic Acid acts as a cushion and lubricant in the joints and other tissues. As we get older, its concentration in our bodies decreases. So I purchased a few bottles of 100 mg Hyaluronic Acid capsules and have been taking one capsule per day for a few weeks. After about a week, my knee and hip pain was reduced to almost zero and has remained that way.
Soon, I think I will cut back my Glucosamine/Chondroitin intake to 1 tablet a day and continue taking the Hyaluronic capsules. If my joint pain returns, I’ll increase the daily Glucosamine/Chondroitin intake back up to 1½ tablet.
Everything else for me remains the same. I continue to use a pillow that prevents pressure on my ears while sleeping, and I still wear face masks or filtered nose plugs when I am above carpeting. I still have no idea what it is in carpeting that causes an inflammation in my trachea when I inhale it for a few minutes. A couple of people have suggested that formaldehyde, in or under the carpeting, could be the problem. That seems plausible to me.
January 8, 2019
On January 2, a very nice couple in the neighborhood invited another neighbor and me over to visit in the afternoon. Then they served us a very tasty dinner. There were three gals (the wife, their neighbor and the neighbor’s girl dog) and three guys (the husband, me and their boy dog). I have this “thing” with other people’s dogs. They usually may not be friendly toward strangers; but within a few minutes of my careful rubbing and gentle scratching, they are my new friends, which usually baffles the owners. That was the case with both dogs, and the smaller dog enjoyed lying in my lap for awhile.There was no carpeting in their house. However, there were large oval rugs in the dining room and living room, where we spent most of our time. Rugs occasionally, but not usually, can be problematic for me. On the other hand, carpeting underneath me causes my trachea to become inflamed and irritated in only a few minutes, if I am not wearing a face mask.
I was there for about 7 hours. During the final 30 miutes or so, I began noticing mild irritation in my trachea. After I went home, the irritation gradually increased, even though I was wearing my mask (due to my carpeting). Within about 30 more minutes, I was coughing and experiencing substantial trachial irritation and pain. Basically, I could not fall asleep. I have not had breathing discomfort and pain like that in a very long time, especially for most of the night. Finally, I got up and took a 40 mg prednisone pill and went back to bed. There was minor improvement after about 30 minutes, but I did not sleep well at all for the rest of the night.
For several days, I have had a frequent runny nose (which is extremely rare for me), deep wet coughing, hard sneezing and pain all the way down my inflamed trachea. Prednisone has helped very little, which it usually does to some extent. I took my temperature today, and it is a couple of degrees higher than normal, which virtually always indicates an infection. I also have had significantly decreased energy, so I have been sitting or lying down quite a bit.
I have been very concerned that my rough coughing and sneezing might rupture my trachea—which has become increasingly brittle over the years due to my RPC—in which case I probably would suffocate before being able to seek medical help, since I would not be getting enough oxygen into my lungs. Even if I were to go to a doctor or a hospital emergency room, there is virtually nothing that can be done to seal up a broken trachea before suffocation occurs, which always is a potential result with RPC.
The neighbor’s wife told me three days ago that she is battling a respiratory infection. She has spent a few days mostly in bed. Nobody was coughing or sneezing at all during our get-together 6 days ago on January 2; however, I have heard that a powerful influenza virus has been infecting many people in the area for a few weeks, so we could have picked it up anywhere. In the past, respiratory infections virtually always have caused my RPC to flare up, and I have to assume that I have a respiratory infection now.
For a few days, I also have been taking 4-5 olive leaf extract capsules, 750 mg each, per 24-hour period, which virtually always has neutralized any infection that I’ve had in 2-3 days. I do not know why there has been no improvement this time, but I am hoping and praying that it will resolve quickly. This is no fun.
January 9, 2019
It seems that my respiratory infection has peaked and now is decreasing. Last night, I got better sleep than I’ve had in several nights. I coughed less, my nose was less runny, I did not sneeze once and my breathing was less uncomfortable.
There still is irritation in my trachea (windpipe), but it is a little less than it was yesterday. When I breathe, especially when I exhale, I can hear rumbling in my breathing passage, and my cough is continuing. I just hope that this infection has not caused significant damage and weakness to my trachea, since a ruptured trachea is the most life-threatening thing that can happen to someone with RPC.
January 20, 2019
I’m still having a semi-persistent dry cough, but that is the only thing remaining from my respiratory infection earlier this month. I also am not hearing anymore rumbling in my trachea when I breathe. So, for now, I seem to be fine.